How Do You Know Your Bladder Is Full
Introduction 
Millions of people in the United States struggle with Overactive Bladder (OAB) symptoms. The most common symptom is the ongoing urgent need to go to the bathroom. Now.
OAB can interfere with work, going out with friends, practise and sleep. Information technology can atomic number 82 you lot to the bathroom many times during the 24-hour interval or dark. Some people leak urine (pee) afterwards this urgent "gotta go" feeling. Others feel afraid they'll leak.
Fortunately, there is help and there are treatments.
What is OAB and Who Gets It? 
Overactive bladder is the name for a grouping of float symptoms. There are three main symptoms:
- A feeling that y'all have to become to the bathroom, urgently.
- Sometimes incontinence, which means that you leak urine with the "gotta go" feeling.
- Normally the need to become to the bathroom often (often), day and nighttime.
With OAB, you lot feel that you need to empty your bladder – even when it's not full. This leads to the feeling that you need a bath rapidly, correct at present. You lot can't command or ignore this feeling. (Although it may feel similar your bladder muscle is squeezing to empty your bladder, in bodily fact your bladder muscle may not be squeezing.) If you "gotta become" eight or more times each day and night, or fear that urine will leak out before you're ready, you may accept OAB.
OAB affects about 33 million Americans. Information technology'south not a normal part of aging. It's a health problem that can final for a long time if it's not treated. Many older men (30%) and women (forty%) struggle with OAB symptoms. Ofttimes people don't know about treatments that can assist, or they don't ask for help.
Stress urinary incontinence or SUI is a different bladder problem. People with SUI leak urine while sneezing, laughing or being active. It is not the aforementioned equally that sudden "gotta get" feeling from OAB. To acquire more nearly SUI, become to https://www.urologymanagement.org/sui/.
In this guide y'all will find articulate information about how to manage OAB. Please ask for help, even if yous feel embarrassed. Don't await, because there are several treatments that work well for OAB. Your health intendance provider should be trained to talk with yous and assistance yous manage your symptoms without embarrassment.
For data nigh the other health care providers trained to help, click here.
How the Urinary Tract Works and What Happens with OAB 
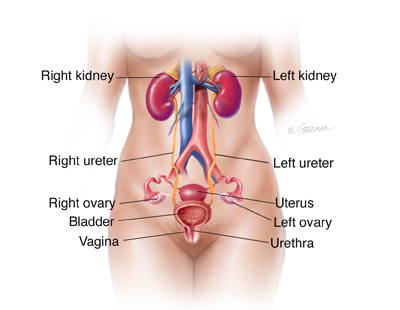
Urinary tract
Medical Illustration Copyright © 2015 Nucleus Medical Media, All rights reserved
The urinary tract is the important system that removes liquid waste from our bodies:
- kidneys: two bean-shaped organs that clean waste from the blood and make urine
- ureters: two thin tubes that accept urine from the kidney to the float
- bladder: a balloon-like sac that holds urine until information technology's time to get to the bath
- urethra: the tube that carries urine from the bladder out of the trunk. The urethra has muscles called sphincters that lock in urine. The sphincters open to release urine when the float contracts.
When your bladder is full, your brain signals the float. The bladder muscles then squeeze. This forces the urine out through the urethra. The sphincters in the urethra open and urine flows out. When your bladder is not full, the bladder is relaxed.
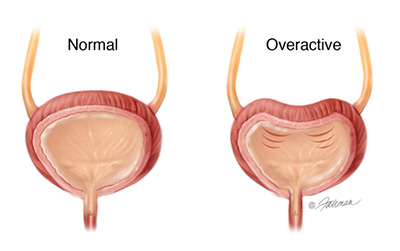
Float and sphincter
Image © 2003 Fairman Studios, LLC
With a healthy float, signals in your brain let you know that your bladder is getting total or is full, simply yous can wait to get to the bathroom. With OAB, you lot can't wait. You lot feel a sudden, urgent need to become. This can happen even if your bladder isn't full.
Symptoms of OAB 
Urgency: This is the primary symptom of OAB. It is a strong (urgent) need to urinate that can't be ignored. This "gotta go" feeling makes people agape that they'll leak urine if they don't find a bath right away. OAB may also cause:
- Incontinence (urine leaks): Sometimes OAB causes urine to leak out before getting to the bathroom. This is called "urgency incontinence." Some people may leak just a few drops, while others can take a sudden gush. (for more than data: https://www.urologyhealth.org/urologic-conditions/urinary-incontinence)
- Urinate oft: OAB may also cause people to go to the bathroom many times during the day. Experts say that "frequent urination" is when you accept to go to the bathroom more than 8 (eight) times in 24 hours.
- Wake up at night to urinate: OAB can wake a person from sleep to go to the bath more once a dark. This is called "nocturia" by health providers.
Some foods and drinks tin bother the bladder. Caffeine, bogus sweeteners, alcohol, chocolate and very spicy foods may make OAB symptoms worse.
OAB does non cause pain. If you feel pain while urinating, you lot may take an infection. Please talk with your health care provider virtually pain.
How OAB Can Bear on Your Life 
Without treatment, OAB symptoms are uncomfortable. Information technology tin be hard to get through the solar day without many visits to the bathroom. OAB tin affect relationships. You may not want to practice things yous bask because you worry near finding a bathroom in time. It can disrupt your slumber and sex life. Information technology can leave you tired and short-tempered, or leaks tin lead to a rash or infections. The whole experience can make anyone feel hopeless and very unhappy.
The good news is that OAB can be controlled. There are treatments bachelor to assistance.
Finding the Words 
Information technology'southward normal to feel uncomfortable when talking about OAB symptoms. Who wants to talk about bathroom issues or incontinence?! Still, knowing more than about OAB is the best manner to have control of the trouble. A niggling planning volition give you confidence. Hither are some tips to help:
- Be prepared: Earlier your appointment, gather useful information to help the health intendance provider learn what's going on. Also be ready to have notes nigh what you learn. Bring:
- A list of the prescription drugs, over-the-counter medicines, vitamins and/or herbs you take.
- A list of your by and electric current illnesses or injuries.
- Results from the Recall You Have Overactive Bladder? Quiz , to assistance you talk over your symptoms.
- A pad of paper and pen to take notes about treatments
- Bring a friend: Ask a close friend or relative to go with y'all to the md, if you lot don't listen sharing what's going on. An "appointment buddy" tin can assist remind yous of things y'all may forget to ask, or remind you of things the health intendance provider said.
- Bring up the topic: If your health intendance provider doesn't enquire about your OAB symptoms, bring up the topic yourself. Don't wait until the end of your visit. Make sure you have time for questions. If a nurse meets with you first, tell the nurse almost your symptoms.
- Speak freely: Share everything you're experiencing. Your health care provider hears about problems every twenty-four hour period. They've heard information technology all! It's OK to tell them about your symptoms and how they affect your daily life. Permit your health care provider know your answers to these questions:
- Exercise my symptoms make me stop doing the things I savour, or foreclose me from going to events?
- Am I afraid to be as well far away from a bathroom?
- Have my symptoms inverse my relationships with friends or family unit?
- Do my symptoms brand information technology hard to get a good dark's sleep?
- Enquire questions: A visit to your health care provider is the right time to ask questions. It is best to bring your list of questions with you so you lot don't forget. We offer some good question to ask in each section of this guide to help you lot.
- Follow-up care: Ask your health care provider when you lot should visit again, and what you should bring with you lot.
How to Diagnose OAB 
When you tell your health care provider about your symptoms, s/he will ask more questions and do some tests. This is done to diagnose the problem. OR, your provider will tell you the name of a specialist who can diagnose and treat you.
To learn what'south happening, a health care provider will probable:
- Inquire nearly your health history: You lot will be asked virtually how you experience, how long y'all've had symptoms, and how they impact you. You will be asked about medicine y'all take (over-the-counter and prescribed). Y'all should also talk nigh what you eat and drink during the twenty-four hours. This lets your provider learn nearly your health at present and in the past.
- Practice a physical exam: Your health care provider will wait for things that could cause symptoms. In men and women, they will feel your organs in and below your belly, in your pelvic area. They will also bank check your rectum.
- Ask y'all to go along a "Bladder Diary:" A Bladder Diary helps you, and your physician, learn about daily events and patterns. In this diary you write down how often you go to the bathroom and if/when you lot leak urine. Yous can apply this Bladder Diary sample to start. You lot can also download an electronic float diary for your mobile device like The Bladder Pal. This app was adult by AUA Member, Dr. Ronald Yap, through the support of the LeBaron Foundation and the Concord Infirmary Trust.
- Bladder Pal app for Android
- Float Pal app for Apple
- Practice other tests if you need them:
- Urine test: a sample of your urine may be tested for infection or blood.
- Bladder scan: This exam shows how much urine is left in your bladder after you go to the bathroom.
- Cystoscopy: Your wellness intendance provider inserts a thin tube with a tiny photographic camera into the bladder to see if it looks normal or not.
- Urodynamic testing: These tests check to meet how well your lower urinary tract holds and lets-go of urine. One of these tests is call CMG (cystometrogram ).
- Symptom quiz: Many doctors use a written quiz to ask questions almost your bladder problems and what causes yous the nearly bother. Take our OAB Quiz
There are a number of things you lot can practise to help manage OAB. Anybody has a different experience with what works all-time. Yous may try ane treatment lonely, or several at the same time. You and your health care provider should talk well-nigh what you lot want from treatment and about each option.
OAB treatments include:
Lifestyle Changes 
To manage OAB, health care providers starting time ask a patient to brand "lifestyle changes". Sometimes these changes are called "behavioral therapy". This could mean that yous consume dissimilar foods, change how much, when or what you beverage, and pre-plan bathroom visits to feel meliorate. Many people notice that these changes help. Other people need to do more than.
- Limit food and drinks that bother your float: Many people feel better when they alter the manner they consume and drink. There are certain foods known to carp the float. Yous can try taking all of these things out of your diet, and then add them back one at a fourth dimension. Once you acquire which foods and drinks make your symptoms worse, yous can avert them. Common foods to avoid:
- Coffee / caffeine
- Tea
- Artificial sweeteners
- Alcohol
- Soda and other fizzy drinks
- Citrus fruit
- Food made with tomatoes
- Chocolate (not white chocolate)
- Spicy foods
- Keep a bladder diary: Writing downwards when y'all make trips to the bathroom for a few days can help you empathise your torso amend. This diary may show you things that make symptoms worse. For instance, are your symptoms worse later on eating or drinking a certain kind of food? Are they worse when you don't drink enough liquids?
- Double voiding (emptying your bladder twice): This may exist helpful for people who have trouble fully emptying their bladders. After you go to the bathroom, you await a few seconds and then endeavor to go again.
- Delayed voiding: This means that y'all practice waiting before y'all go to the bath, even when you have to become. At first, y'all wait only a few minutes. Gradually you may be able to wait ii to three hours at a time. Merely endeavour this if your health intendance provider tells you lot to. Some people feel worse or have urine leaks when they wait too long to become to the bathroom.
- Timed urination: This means that you follow a daily bath schedule. Instead of going when yous feel the urge, you get at ready times during the day. You and your health care provider will create a reasonable schedule. You may try to urinate every two to four hours, whether you feel yous have to become or not. The goal is to prevent that "urgent" feeling and to gain control.
- Exercises to relax your bladder muscle: You may be familiar with exercises to strengthen your pelvic flooring muscles, besides called Kegel exercises. A special do using those same pelvic flooring muscles may assist relax your bladder during those "gotta go" moments. To do "quick flicks," you lot speedily clasp and relax your pelvic floor muscles repeatedly. When you experience the urge to get, attempt a number of "quick flicks" instead. These exercises tin help control that "gotta go" feeling. It helps to exist still, relax and focus on just the exercise. Your wellness care provider or a concrete therapist can help you learn these exercises. Biofeedback may also help. Biofeedback uses computer graphs and sounds to monitor musculus movement. Information technology can help teach you how your pelvic muscles move and how strong they are.
Prescription Drugs 
When lifestyle changes aren't enough, the adjacent step may be to take medicine. Your health care provider can tell you about special drugs for OAB.
At that place are several types that can relax the bladder muscle. These drugs (for example: Anti-muscarenics and Beta-3 agonists) can help finish your bladder from squeezing when information technology's not total. Some are taken every bit pills, past mouth. Others are gels or a glutinous patch to give you the drug through your skin.
Your wellness intendance provider will want to know if the medicine works for you. They will bank check to see if you get relief or if the drug causes problems, known as "side-effects". Some people become dry mouth and dry eyes, constipation, or blurred vision.
To help relieve symptoms, your health care provider may ask you to take different amounts of the drug. Or, requite yous a different 1 to try. You may be asked to make lifestyle changes and take medicine at the aforementioned time for amend results.
Injections 
If lifestyle changes and medicine aren't working, there are other options. A trained urologist or FPMRS specialist tin can help. They may offer float injections (shots) of Botox® (botulinum toxin).
Minor amounts of Botox® can stop the bladder muscles from squeezing besides much. Many tiny injections are used. It gently paralyzes the muscles. Additional treatments are given when this handling wears off, anywhere from six to twelve months later. Your doctor will watch how you're doing to make sure you aren't retaining (holding in) too much urine. If urine is not draining well, you may need to catheterize temporarily.
Nervus Stimulation (Neuromodulation Therapy) 
Another treatment for people who need extra assist is nervus stimulation, too called neuromodulation [pronounced: NER-oh-mahd-yoo-LAY-shun] therapy.
This type of treatment sends electrical pulses to nerves in your bladder. In OAB, the nerve signals between your float and brain don't piece of work the right way. These electrical pulses interrupt the nerve signals, set them right, and improve OAB symptoms.
There are two types:
- Sacral neuromodulation (SNS) changes how the sacral nerve works. This nerve carries signals between the spinal cord and the bladder. Its job is to help hold and release urine. In OAB, these nerve signals aren't doing what they should. SNS uses a "float pacemaker" to control these signals to finish OAB symptoms. SNS is a two-step surgical process. The starting time step is to implant an electrical wire nether the skin in your lower back. This wire is first connected to a handheld "pacemaker" to send pulses to the sacral nerve. You and your doctor volition test whether or not this pacemaker can aid you. If it helps, the 2d pace is to implant a permanent pacemaker that tin can regulate the nerve rhythm.
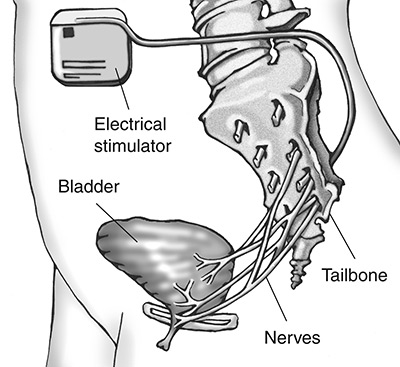
Sacral neuromodulation (SNS)
National Constitute of Diabetes and Digestive and Kidney Diseases,
National Institutes of Health - Percutaneous tibial nerve stimulation (PTNS) is another mode to right the nerves in your bladder. For this blazon of nerve stimulation you will not have to have surgery. PTNS is performed during an office visit that takes almost 30 minutes. PTNS is done past placing a small electrode in your lower leg almost your talocrural joint. It sends pulses to the tibial nerve. The tibial nervus runs along your knee to the sacral nerves in your lower back. The pulses assistance control the signals that aren't working right. Often, patients receive 12 treatments, depending on how it's working. [This therapy is pronounced: PER-cyoo-TAY-nee-uhs TI-bee-ahl NERV STIM-yoo-LAY-shun.]
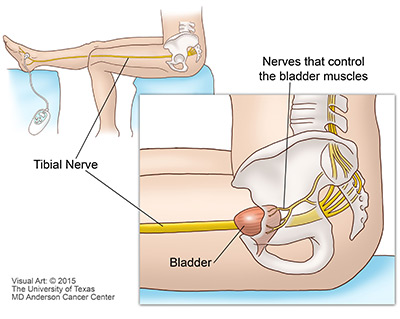
Percutaneous tibial nerve stimulation (PTNS)
(c)2012 The University of Texas M.D. Anderson Cancer
Other Resources 
Hither are a few more organizations that offer useful information to aid people living with OAB and incontinence.
Urology Intendance Foundation
1-800-828-7866
The official foundation of the American Urological Association, the Urology Care Foundation is committed to advancing urologic inquiry and education. We collaborate with researchers, wellness care providers, patients and caregivers to improve patients' lives.
American Urological Association
The American Urological Association promotes the highest standards of urological clinical intendance through education, research and health care policy.
Information technology's Time to Talk about OAB
Get the facts. Get diagnosed. Have control.
Order printed materials most OAB, take our "Overactive Bladder Quiz," and download a "Float Diary" to rail your symptoms.
Information technology's Time to Talk about SUI
Detect out more than about Stress Urinary Incontinence, society printed materials and take the SUI quiz.
National Kidney and Urologic Diseases Clearinghouse:
The National Kidney and Urologic Diseases Data Clearinghouse (NKUDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) that provides information on kidney and urologic diseases. The NIDDK is part of the U.South. National Institutes of Wellness (NIH).
National Clan for Continence
The National Clan for Continence is a national, private, not-turn a profit system dedicated to improving the quality of life of people with incontinence, voiding dysfunction, and related pelvic flooring disorders. NAFC'due south purpose is to be the leading source for public pedagogy and advocacy near the causes, prevention, diagnosis, treatments, and management alternatives for incontinence.
Simon Foundation for Continence
The mission of the Simon Foundation is to bring the topic of incontinence out into the open, remove the stigma surrounding incontinence, and provide help and hope to people with incontinence, their families and the health professionals who provide their care.
Patient resources provided through the generous back up of:

Source: https://www.urologyhealth.org/overactive-bladder
0 Response to "How Do You Know Your Bladder Is Full"
Postar um comentário